**If you would like another chance to read the challenge before seeing the answer, click here. Scroll down for the answer. **
———————————————————————————————————————————————————————————–
Let me begin by saying this was a difficult case (I know a case is tricky when the ratio of views to answers is >400:1), and kudos to those who tried – the history really forces you to keep inflammatory bowel disease, infectious colitis, and antibiotic-associated/C. diff colitis on the differential.
Radiology key for this case:
Given the patient’s acute presentation, history of bathroom and fresh-water lake swimming, recent antibiotic use, and his illness’ self-limited nature & response to antibiotics, the most likely etiology is E) Infectious colitis; specifically, I felt this patient had a presentation consistent with amoebiasis, but unfortunately, only a single stool sample was collected, and although the diagnosis can be clinched with ova & parasite screening, this test is only 30-50% sensitive for a single stool sample. A more sensitive (>90%) stool antigen test exists, but was not ordered.
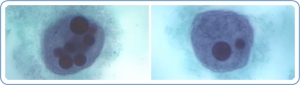
Trophozoite forms of E. histolytica containing multiple ingested red blood cells. Image credit: CDC.
Amoebiasis is a parasitic infection caused by Entamoeba histolytica, and is estimated to cause 70,000-100,000 deaths per year, worldwide. It is more common in people who live in tropical areas or where sanitary conditions are poor, but does occur in the US. It causes a mild to severe colitis, but only 10-20% of those infected become symptomatic. The incubation period varies, but most infected persons become symptomatic between 2-4 weeks of inoculation. Invasion of the intestinal/colonic wall (causing characteristic “flask-shaped” ulcerations) precedes symptoms, and is the cause of bloody stools. Fever is uncommon.
E. histolytica is sensitive to metronidazole, among other antibiotics.
The patient’s presentation, hospital course, and response to metronidazole are also consistent with “antibiotic-associated” or C. difficile colitis, but a negative PCR (high sensitivity) as well as low risk of colonization in this patient make the diagnosis fairly unlikely. C. difficile colitis is also associated with markedly high WBC counts, a characteristic foul-smelling/malodorous diarrhea (with or without blood), and pseudomembranes on colonoscopy.

C. difficile pseudomembranous colitis. Image credit: Medscape
Other bacterial agents such as Campylobacter and E. coli should also be considered.
Explanations
Choice A) Food poisoning is not the best answer because while patients present acutely and do have abdominal pain and anorexia, they commonly present with acute-onset nausea & vomiting, though diarrhea alone can be present. This patient gives no history of dietary changes, barbeques, or questionably-prepared food, and has no known sick contacts. Additionally, bloody stools would not be expected.
Choice B) Microscopic colitis is wrong because, by default, these patients have no visible signs of colitis, except on microscopy. Chronic, watery diarrhea, abdominal pain, and weight loss are common. It is mostly diagnosed in middle-aged Caucasians, with a 3:1 female predominance, and is associated with celiac disease, irritable bowel syndrome, and autoimmune thyroid disease. Two varieties, lymphocytic colitis & collagenous colitis, exist, and are distinguished on microscopic examination of the colon.
Answers C) & D) (Crohn’s disease & ulcerative colitis) are unlikely because although patients do present with abdominal pain and diarrhea with blood and/or mucus, and this patient does have a positive family history, his presentation is rather acute in nature, and the self-limited course and response to antibiotics are uncharacteristic of such a severe inflammatory bowel disease (IBD) flare-up. Ulcerative colitis almost always involves the rectum, and fevers & weight loss are common in Crohn’s disease; other extra-intestinal symptoms may help the clinician diagnose IBD. Corticosteroids, anti-inflammatory medications, and immune-modulating drugs are the main treatments employed.
Thanks for participating. If you would like to submit a case or guest post, please use the contact page.


Posted on August 21, 2012
0